Diagnosing Metastatic Spread Outside the Prostate
Overview by Dr Tristan Barrett
Consultant Radiologist
Department of Radiology
University of Cambridge School of Clinical Medicine

Diagnosing metastatic prostate cancer
Accurate staging of prostate cancer is essential to inform prognosis and to stratify patients for appropriate management both at initial presentation, or in the context of suspected recurrent or progressive disease. When prostate cancer metastasises, that is it spreads outside of the prostate gland, it typically affects areas and structures in the immediate vicinity of the prostate gland such as the pelvic lymph nodes, bladder and the seminal vesicles. The spread of disease is classified according to the TNM staging system:
Nodal spread is primarily to four pelvic areas, considered regional nodes: the obturator, internal and external iliac and pre-sacral nodes. When distal metastatic involvement is present, the common site is bone (in >80%), with involvement of other organs occurring in around 10%, which may include liver, lungs, brain. Clinically low stage disease i.e. PSA <10 ng/ml, or Gleason grade <7, or stage ≤T2a, has a low probability of metastases, thus additional imaging tests are not recommended for staging. Current EAU guidelines recommend cross-sectional abdominopelvic imaging (CT or MRI) and bone-scintigraphy for metastatic screening in patients with predominantly Gleason pattern 4 disease or higher (i.e. Grade Group ≥3).
Diagnosing metastatic spread
mpMRI scans
Locally advanced disease, or “T-staging” is determined by an mpMRI scan which would have initially been performed when prostate cancer was suspected.
Symptoms and signs that may indicate prostate cancer spread include lower back pain, which might be the result of bone metastases in the lower spine, and an elevation in liver function enzymes, indicating spread to the liver. Any of these indicators of potential metastases should trigger further investigation.
As well as being the diagnostic tool for prostate cancer confined to the gland itself, it has an incremental value in assessing pelvic nodal disease and bone involvement. mpMRI scans may also be appropriate when PSA is rising rapidly post surgery to determine if there is local recurrance of disease, or local spread as already described.
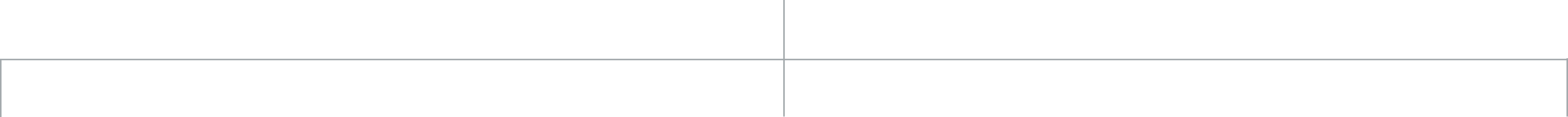
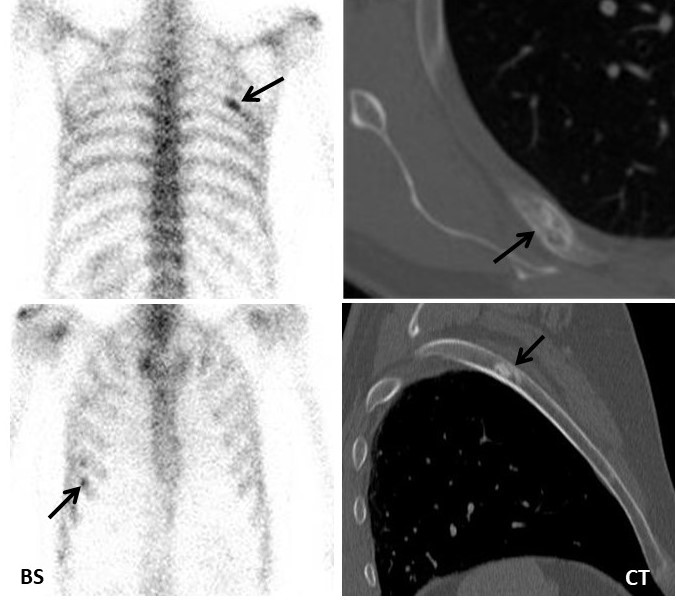
Bone scintigraphy
Bone scintigraphy, also known as a bone scan, uses a radiotracer (a small amount of radioactive material) that is injected into the bloodstream. The radiotracer travels through the bloodstream and will usually be seen in higher concentration in areas of bone with metastatic involvement. These areas appear as ‘hot spots’ on the scan, with the radiation emitted being detected by a gamma camera. The images are then computed to create images of bones. However false positives are not uncommon, wherein ‘hot spots’ are seen on the scan which are not related to prostate cancer cells.
CT scans
CT scans can be used to locate prostate cancer that has spread to the liver, intestines, or bones of the abdomen and pelvis. Cancer which has spread to the lymph nodes can also be detected if the lymph nodes have become enlarged. The normal size range of lymph nodes varies by anatomical region. Nodes are considered abnormal with a short axis dimeter of >8 mm in the pelvis and >10 mm outside the pelvis, however, this size threshold has poor sensitivity for detecting metastatic involvement; decreasing these thresholds improves sensitivity but reduces specificity, thus size threshold alone remains sub-optimal.
Examples of Bone and CT scans are shown below. the arrows indicate cancer location.
Next Generation Imaging
“Next generation imaging” for prostate cancer is a broad term which incorporates imaging techniques to stage prostate cancer beyond conventional imaging with bone scintigraphy and CT. Techniques include whole- body (WB) MRI and Positron Emission Tomography (PET) imaging using different radiotracers. The RADAR (Radiographic Assessments for Detection of Advanced Recurrence) Group recently recommended that next generation imaging techniques should be used in select patients in whom conventional imaging is equivocal or negative for metastatic involvement, but considered at high clinical risk based on laboratory (biomarker) values, comorbidities and/or symptoms.
WB-MRI incorporates anatomical and functional imaging with coverage from head-to-thighs, and is particularly accurate in assessment of bone disease. The diagnostic accuracy of WB-MRI is much higher than that of bone scintigraphy; with equal staging accuracy to choline PET/CT.
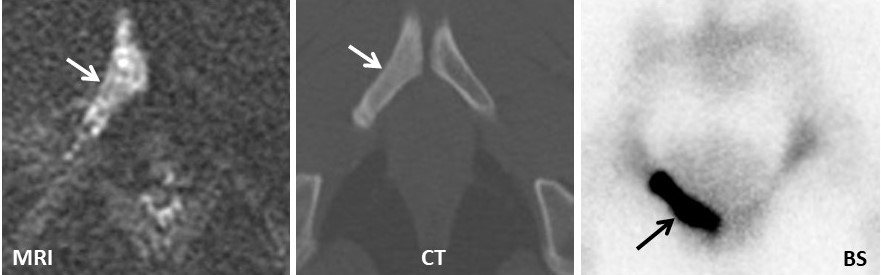
PET imaging can be combined with MRI, or more typically CT. There are several potential radiotracers available, with the most common in clinical practice being choline and prostate specific membrane antigen (PSMA). PSMA is a protein on the surface cells in the prostate gland, with prostate cancer cells usually expressing more PSMA than normal cells wherever they are in the body, even if they have metastasised.. For diagnostic purposes, PSMA is linked to either radioactive Gallium-68 or Fluorine-18, with the primary tumour or metastatic spread being seen as hot spots on the scan. PSMA can also be linked to the radioactive tracer Lutetium-177, which can be used for the dual purpose of imaging for diagnosis and radiotherapy for treatment, a technique known as theranostic therapy. See link. PET-CT images are shown below.

Prostate matters is a not for profit organisation that is committed to providing free expert advice about prostate issues from leading Clinical Authorities
PROSTATE MATTERS
FOLLOW US
Copyright Disclaimer: We try to acknowledge copyright as appropriate. If we have used something without acknowledging copyright, this is inadvertent. Please let us know by emailing info@prostatematters.co.uk